The transient receptor potential cation channel subfamily V member 1 (TRPV1), also known as the capsaicin receptor and the vanilloid receptor 1, is a protein that, in humans, is encoded by the TRPV1 gene. It was the first isolated member of the transient receptor potential vanilloid receptor proteins that in turn are a sub-family of the transient receptor potential protein group.[5][6] This protein is a member of the TRPV group of transient receptor potential family of ion channels.[7] Fatty acid metabolites with affinity for this receptor are produced by cyanobacteria, which diverged from eukaryotes at least 2000 million years ago (MYA).[8] The function of TRPV1 is detection and regulation of body temperature. In addition, TRPV1 provides a sensation of scalding heat and pain (nociception). In primary afferent sensory neurons, it cooperates with TRPA1[9][10] (a chemical irritant receptor) to mediate the detection of noxious environmental stimuli.[11]
Function
editTRPV1 is an element of or mechanism used by the mammalian somatosensory system.[12] It is a nonselective cation channel that may be activated by a wide variety of exogenous and endogenous physical and chemical stimuli. The best-known activators of TRPV1 are: temperature greater than 43 °C (109 °F); acidic conditions; capsaicin (the irritating compound in hot chili peppers); and allyl isothiocyanate, the pungent compound in mustard and wasabi.[13] The activation of TRPV1 leads to a painful, burning sensation. Its endogenous activators include: low pH (acidic conditions), the endocannabinoid anandamide, N-oleyl-dopamine, and N-arachidonoyl-dopamine. TRPV1 receptors are found mainly in the nociceptive neurons of the peripheral nervous system, but they have also been described in many other tissues, including the central nervous system. TRPV1 is involved in the transmission and modulation of pain (nociception), as well as the integration of diverse painful stimuli.[14][15]
Sensitization
editThe sensitivity of TRPV1 to noxious stimuli, such as high temperatures, is not static. Upon tissue damage and the consequent inflammation, a number of inflammatory mediators, such as various prostaglandins and bradykinin, are released. These agents increase the sensitivity of nociceptors to noxious stimuli. This manifests as an increased sensitivity to painful stimuli (hyperalgesia) or pain sensation in response to non-painful stimuli (allodynia). Most sensitizing pro-inflammatory agents activate the phospholipase C pathway. Phosphorylation of TRPV1 by protein kinase C has been shown to play a role in sensitization of TRPV1. The cleavage of PIP2 by PLC-beta can result in disinhibition of TRPV1 and, as a consequence, contribute to the sensitivity of TRPV1 to noxious stimuli.
Desensitization
editUpon prolonged exposure to capsaicin, TRPV1 activity decreases, a phenomenon called desensitization. Extracellular calcium ions are required for this phenomenon, thus influx of calcium and the consequential increase of intracellular calcium mediate this effect.[16] Various signaling pathways such as phosphorylation by PKA and PKC, interaction with calmodulin, dephosphorylation by calcineurin,[17] and the decrease of PIP2, have been implicated in the regulation of desensitization of TRPV1. Desensitization of TRPV1 is thought to underlie the paradoxical analgesic effect of capsaicin.
Clinical significance
editPeripheral nervous system
editAs a result of its involvement in nociception, TRPV1 has been a target for the development of pain reducers (analgesics). Three major strategies have been used:
TRPV1 use
editThe TRPV1 receptor can be used to measure how an organism can sense temperature change. In the lab the receptor may be removed from mice giving them the inability to detect differences in ambient temperature. In the pharmaceutical field this allows for the blocking of heat receptors giving patients with inflammatory disorders or severe burning pains a chance to heal without the pain. The lack of the TRPV1 receptor gives a glimpse into the developing brain as heat can kill most organisms in large enough doses, so this removal process shows researchers how the inability to sense heat may be detrimental to the survivability of an organism and then translate this to human heat disorders.[citation needed]
TRPV1 in immune cells
editTRPV1 plays an important role not only in neurones but also in immune cells. Activation of TRPV1 modulates immune response including the release of inflammatory cytokines, chemokines, and the ability to phagocytose. However, the role of TRPV1 in immune cells is not entirely understood and it is currently intensely studied. TRPV1 is not the only TRP channel expressed in immune cells. TRPA1, TRPM8 and TRPV4 are the most relevant TRP channels that are also studied in immune cells.[18]
The expression of TRPV1 was confirmed in the cells of innate immunity as well as the cells of adaptive immunity. TRPV1 can be found in monocytes, macrophages, dendritic cells, T lymphocytes, natural killer cells and neutrophiles.[19] TRPV1 is said to be potentially very important in immune cell functioning as it senses higher temperature and lower pH, which can affect the immune cell performance.[20]
TRPV1 and adaptive immunity
editTRPV1 is an important membrane channel in T cells as it regulates the influx of calcium cations. TRPV1's involvement is mainly in T cell receptor signalling (TCR) signalling, T cell activation and TCR-mediated influx of calcium ions,[19] but it is involved in T cell cytokine production as well.[20] Indeed, T cells with TRPV1 knockout show impaired calcium uptake after T cell activation via TCR, thus they show dysregulation in signalling pathways such as NF-κB and NFAT.[18]
TRPV1 and innate immunity
editRegarding innate immunity, activation of TRPV1 by capsaicin has been shown to suppress the production of nitrite radical, superoxide anion and hydrogen peroxide by macrophages. Furthermore, administration of capsaicin, and subsequent activation of TRPV1, suppresses phagocytosis in dendritic cells. In a mouse model, TRPV1 affect dendritic cell maturation and function, however, further studies are needed to clarify this effect in humans. In neutrophils, the increase in cytosolic calcium cations leads to synthesis of prostaglandins. Activation of TRPV1 by capsaicin modulates neutrophil immune response due to the higher influx of calcium ions into the cell.[19]
TRPV1 is also considered a novel therapeutic agent in many inflammatory diseases. Multiple studies have proven that TRPV1 influences the outcome of several inflammatory diseases such as chronic asthma, esophageal inflammation, rheumatoid arthritis and cancer. Studies using TRPV1's agonists and antagonists have shown that their administration indeed changes the course of inflammation. However, at this point, there is a lot of contradictive evidence about what type of response, pro-inflammatory or anti-inflammatory, TRPV1's activation induces. Further research needs to be carried out. Meanwhile, it is important to highlight that TRPV1's influence on inflammatory diseases is probably not limited to only immune cells as it is rather an interplay between immune cells, neurons, and other cell types (epithelial cells etc.).[20]
TRPV1 and cancer
editTRPV1 was found to be overexpressed in several types of cancers, e.g., pancreatic cancer and colon adenocarcinoma. This suggest that certain types of cancers might be more prone to cell death mediated by capsaicin-induced (and also other vanilloid-induced) cell death. Indeed, studies have shown inversed correlation of consumption of chili-based foods and all-cause mortality along with cancers. This beneficial impact of the consumption of chili-based foods was attributed to capsaicinoid content.[19]
TRPV1 activation caused by its agonist capsaicin was shown to induce G0-G1 cell arrest and apoptosis in leukemic cell lines, adult T-cell leukaemia and multiple myeloma. Capsaicin reduces the expression of anti-apoptotic protein Bcl-2 and it also promotes activation of p53, a tumour-suppressor protein known as a major regulator of cell death. This effect of capsaicin in both cases subsequently leads to above-mentioned apoptosis.[19]
TRPV1 and neuroinflammation
editThe interplay between neurons and immune cells is a well-known phenomenon.[21] TRPV1 plays its role in neuroinflammation, being expressed both in neurons and in immune cells. Significant importance should be paid to the confirmed expression of TRPV1 in microglia and astrocytes, cells found close to neurons. The neuro-immune axis is the place of production of neuroinflammatory molecules and receptors that interplay between the two systems and ensure a complex response to external stimuli (or to the body's own pathologies). Studying TRPV1's involvement in neuroinflammation has a great therapeutical significance for the future.[22]
Cutaneus neurons expressing TRPV1 and dendritic cells were found to be located close to each other. Activation of TRPV1 channels in neurons is associated with subsequent production of interleukin 23 (IL-23) by dendritic cells and further production of IL-17 by T cells. These interleukins are important for host defence against pathogenic fungi (such as Candida albicans) and bacteria (such as Staphylococcus aureus), thus TRPV1's activation can lead to better defence against these pathogens, thanks to the neuro-immune axis.[20]
TRPV1 is said to contribute to autophagy of microglia via its Ca2+-signalling, which leads to mitochondria-induced cell death. The TRPV1 channel also influences microglia-induced inflammation. Migration and chemotaxis of microglia and astrocytes seems to be affected by TRPV1's interaction with the cytoskeleton and Ca2+-signalling. TRPV1 is therefore involved in the neuro-immune axis via its function in microglia as well.[22]
TRPV1 was shown to have protective effect in neurologic disorders such as Huntington's disease, vascular dementia, and Parkinson's disease. However, its precise function needs to be further explored.[22]
Ligands
editAntagonists
editAntagonists block TRPV1 activity, thus reducing pain. Identified antagonists include the competitive antagonist capsazepine and the non-competitive antagonist ruthenium red. These agents could be useful when applied systemically.[23] Numerous TRPV1 antagonists have been developed by pharmaceutical companies. TRPV1 antagonists have shown efficacy in reducing nociception from inflammatory and neuropathic pain models in rats.[24] This provides evidence that TRPV1 is capsaicin's sole receptor. [25] In humans, drugs acting at TRPV1 receptors could be used to treat neuropathic pain associated with multiple sclerosis, chemotherapy, or amputation, as well as pain associated with the inflammatory response of damaged tissue, such as in osteoarthritis.[26]
These drugs can affect body temperature (hyperthermia) which is a challenge to therapeutic application. For example, a transient temperature gain (~1 °C for a duration of approximately 40 minutes, reverting to baseline by 40 minutes) was measured in rats with the application of TRPV1 antagonist AMG-9810.[27] The role of TRPV1 in the regulation of body temperature has emerged in the last few years. Based on a number of TRPV-selective antagonists' causing a mild increase in body temperature (hyperthermia), it was proposed that TRPV1 is tonically active in vivo and regulates body temperature[27] by telling the body to "cool itself down". Without these signals, the body overheats. Likewise, this explains the propensity of capsaicin (a TRPV1 agonist) to cause sweating (i.e.: a signal to reduce body temperature). In a recent report, it was found that tonically active TRPV1 channels are present in the viscera and keep an ongoing suppressive effect on body temperature.[28] Recently, it was proposed that predominant function of TRPV1 is body temperature maintenance.[29] Experiments have shown that TRPV1 blockade increases body temperature in multiple species, including rodents and humans, suggesting that TRPV1 is involved in body temperature maintenance.[27] In 2008, AMG-517, a highly selective TRPV1 antagonist was dropped out of clinical trials due to the causation of hyperthermia (~38.3 °C mean increase which was most intense on day 1 but was attenuated on days 2–7.[30] Another molecule, SB-705498, was also evaluated in the clinic but its effect on body temperature was not reported.[31][32] As we increase understanding of modality specific agonism of TRPV1 it seems that next generation therapeutics targeting TRPV1 have the potential to side-step hyperthermia.[33] Moreover, for at least two indications or approaches this may be a secondary issue. Where the therapeutic approach (e.g., in analgesia) is agonist-mediated desensitization then the hyperthermic effects of antagonists may not be relevant. Secondarily in applications such as TRPV1 antagonism for the treatment of severe conditions such as heart failure, then there may be an acceptable trade-off with mild hyperthermia, although no hyperthermia was observed in rodent models of heart failure treated with BCTC, SB-366791 or AMG-9810.[34][35] Post translational modification of TRPV1 protein by its phosphorylation is critical for its functionality. Reports published from NIH suggest that Cdk5-mediated phosphorylation of TRPV1 is required for its ligand-induced channel opening.[36]
Agonists
editTRPV1 is activated by numerous agonists from natural sources.[37] Agonists such as capsaicin and resiniferatoxin activate TRPV1 and, upon prolonged application, cause TRPV1 activity to decrease (desensitization), leading to alleviation of pain via the subsequent decrease in the TRPV1 mediated release of inflammatory molecules following exposures to noxious stimuli. Agonists can be applied locally to the painful area in various forms, generally as a patch or an ointment. Numerous capsaicin-containing creams are available over the counter, containing low concentrations of capsaicin (0.025 - 0.075%). It is debated whether these preparations actually lead to TRPV1 desensitization; it is possible that they act via counter-irritation. Novel preparations containing higher capsaicin concentration (up to 10%) are under clinical trials.[38] Eight percent capsaicin patches have recently become available for clinical use, with supporting evidence demonstrating that a 30-minute treatment can provide up to 3 months analgesia by causing regression of TRPV1-containing neurons in the skin.[39] Currently, these treatments must be re-administered on a regular (albeit infrequent) schedule in order to maintain their analgesic effects.
Cannabinoid ligands
editCannabinoid ligands include:[40]
- Cannabidiol (CBD) – agonist[41]
- Cannabigerol (CBG) – agonist [42]
- Tetrahydrocannabivarin (THCV) – agonist [43]
- Cannabigerovarin (CBGV) – agonist [43]
N-Acyl amides
editN-Acyl Amides that activate cannabimimetic receptors include:[40]
- Anandamide (AEA) [44]
- N-Arachidonoyl dopamine[45]
- N-Oleoyl dopamine [46]
- N-Arachidonoyl taurine [47]
- N-Docosahexaenoyl ethanolamine [48]
- N-Docosahexaenoyl GABA [48]
- N-Docosahexaenoyl aspartic acid [48]
- N-Docosahexaenoyl glycine [48]
- N-Docosahexaenoyl serine [48]
- N-Arachidonoyl GABA [48]
- N-Linoleyl GABA [48]
Fatty acid metabolites
editCertain metabolites of polyunsaturated fatty acids have been shown to stimulate cells in a TRPV1-dependent fashion. The metabolites of linoleic acid, including 13(S)-hydroxy-9Z,11E-octadecadienoic acid (13(S)-HODE), 13(R)-hydroxy-9Z,11E-octadecadienoic acid (13(R)-HODE, 9(S)-hydroxy-10(E),12(Z)-octadecadienoic acid (9(S)-HODE), 9(R)-hydroxy-10(E),12(Z)-octadecadienoic acid (9(R)-HODE), and their respective keto analogs, 13-oxoODE and 9-oxoODE (see 13-HODE and 9-HODE sections on Direct actions), activate peripheral and central mouse pain sensing neurons. Reports disagree on the potencies of these metabolites with, for example, the most potent one, 9(S)-HODE, requiring at least 10 micromoles/liter.[49] or a more physiological concentration of 10 nanomoles/liter[50] to activate TRPV1 in rodent neurons. The TRPV1-dependency of these metabolites' activities appears to reflect their direct interaction with TPRV1. Although relatively weak agonists of TRPV1 in comparison to anandamide,[49] these linoleate metabolites have been proposed to act through TRPV1 in mediating pain perception in rodents[50][51][52] and to cause injury to airway epithelial cells and thereby to contribute to asthma disease[53] in mice and therefore possibly humans. Certain arachidonic acid metabolites, including 20-hydroxy-5Z,8Z,11Z,14Z-eicosatetraenoic acid (see 20-Hydroxyeicosatetraenoic acid)[54] and 12(S)-hydroperoxy-5Z,8Z,10E,12S,14Z-eicosatetraenoic acid (12(S)-HpETE), 12(S)-hydroxy-5Z,8Z,10E,12S,14Z-eicosatetraenoic acid (12(S)-HETE (see 12-HETE), hepoxilin A3 (i.e. 8R/S-hydroxy-11,12-oxido-5Z,9E,14Z-eicosatrienoic acid) and HxB3 (i.e. 10R/S-hydroxy-11,12-oxido-5Z,8Z,14Z-eicosatrienoic acid) likewise activate TRPV1 and may thereby contribute to tactile hyperalgesia and allodynia (see Hepoxilin § Pain perception).[55][56][57]
Studies with mice, guinea pig, and human tissues and in guinea pigs indicate that another arachidonic acid metabolite, Prostaglandin E2, operates through its prostaglandin EP3 G protein coupled receptor to trigger cough responses. Its mechanism of action involves activation and/or sensitization of TRPV1 (as well as TRPA1) receptors, presumably by an indirect mechanism. Genetic polymorphism in the EP3 receptor (rs11209716[58]), has been associated with ACE inhibitor-induced cough in humans.[59][60]
Resolvin E1 (RvE1), RvD2 (see resolvins), neuroprotectin D1 (NPD1), and maresin 1 (Mar1) are metabolites of the omega 3 fatty acids, eicosapentaenoic acid (for RvE1) or docosahexaenoic acid (for RvD2, NPD1, and Mar1). These metabolites are members of the specialized proresolving mediators (SPMs) class of metabolites that function to resolve diverse inflammatory reactions and diseases in animal models and, it is proposed, humans. These SPMs also dampen pain perception arising from various inflammation-based causes in animal models. The mechanism behind their pain-dampening effects involves the inhibition of TRPV1, probably (in at least certain cases) by an indirect effect wherein they activate other receptors located on the neurons or nearby microglia or astrocytes. CMKLR1, GPR32, FPR2, and NMDA receptors have been proposed to be the receptors through which these SPMs operate to down-regulate TRPV1 and thereby pain perception.[61][62][63][64][65]
Fatty acid conjugates
editN-Arachidonoyl dopamine, an endocannabinoid found in the human CNS, structurally similar to capsaicin, activates the TRPV1 channel with an EC50 of approximately of 50 nM.[15]
N-Oleyl-dopamine, another endogenous agonist, binds to human VR1 with an Ki of 36 Nm.[66]
Another endocannabinoid anandamide has also been shown to act on TRPV1 receptors.[67]
AM404—an active metabolite of paracetamol (also known as acetaminophen)—that serves as an anandamide reuptake inhibitor and COX inhibitor also serves as a potent TRPV1 agonist.[68]
The plant-biosynthesized cannabinoid cannabidiol also shows "either direct or indirect activation" of TRPV1 receptors.[69][42] TRPV1 colocalizes with CB1 receptors and CB2 receptors in sensory and brain neurons respectively, and other plant-cannabinoids like CBN, CBG, CBC, THCV, and CBDV are also agonists of this ion channel.[70][69] There is also evidence that non cannabinoid components of the Cannabis secondary metabolome such as myrcene activate TRPV1.[71]
Vitamin D metabolites
editThe vitamin D metabolites calcifediol (25-hydroxy vitamin D or 25OHD) and calcitriol (1,25-hydroxy vitamin D or 1,25OHD) act as endogenous ligands of TRPV1.[72]
Central nervous system
editTRPV1 is also expressed at high levels in the central nervous system and has been proposed as a target for treatment not only of pain but also for other conditions such as anxiety.[73] Furthermore, TRPV1 appears to mediate long-term synaptic depression (LTD) in the hippocampus.[74] LTD has been linked to a decrease in the ability to make new memories, unlike its opposite long-term potentiation (LTP), which aids in memory formation. A dynamic pattern of LTD and LTP occurring at many synapses provides a code for memory formation. Long-term depression and subsequent pruning of synapses with reduced activity is an important aspect of memory formation. In rat brain slices, activation of TRPV1 with heat or capsaicin induced LTD while capsazepine blocked capsaicin's ability to induce LTD.[74] In the brainstem (solitary tract nucleus), TRPV1 controls the asynchronous and spontaneous release of glutamate from unmyelinated cranial visceral afferents - release processes that are active at normal temperatures and hence quite distinct from TRPV1 responses in painful heat.[75] Hence, there may be therapeutic potential in modulating TRPV1 in the central nervous system, perhaps as a treatment for epilepsy (TRPV1 is already a target in the peripheral nervous system for pain relief).
Interactions
editTRPV1 has been shown to interact with:
Discovery
editThe dorsal root ganglion (DRG) neurons of mammals were known to express a heat-sensitive ion channel that could be activated by capsaicin.[79] The research group of David Julius, therefore, created a cDNA library of genes expressed in dorsal root ganglion neurons, expressed the clones in HEK 293 cells, and looked for cells that respond to capsaicin with calcium influx (which HEK-293 normally do not). After several rounds of screening and dividing the library, a single clone encoding the TRPV1 channel was finally identified in 1997.[5] It was the first TRPV channel to be identified. Julius was awarded the 2021 Nobel prize in Physiology or Medicine for his discovery.
See also
editReferences
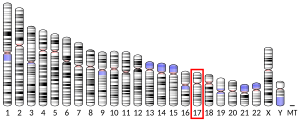
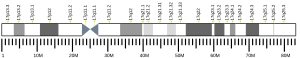
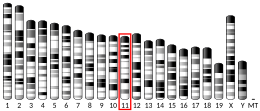
edit- ^ a b c GRCh38: Ensembl release 89: ENSG00000196689 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000005952 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D (October 1997). "The capsaicin receptor: a heat-activated ion channel in the pain pathway". Nature. 389 (6653): 816–824. Bibcode:1997Natur.389..816C. doi:10.1038/39807. PMID 9349813. S2CID 7970319.
- ^ Xue Q, Yu Y, Trilk SL, Jong BE, Schumacher MA (August 2001). "The genomic organization of the gene encoding the vanilloid receptor: evidence for multiple splice variants". Genomics. 76 (1–3): 14–20. doi:10.1006/geno.2001.6582. PMID 11549313.
- ^ Clapham DE, Julius D, Montell C, Schultz G (December 2005). "International Union of Pharmacology. XLIX. Nomenclature and structure-function relationships of transient receptor potential channels". Pharmacological Reviews. 57 (4): 427–450. doi:10.1124/pr.57.4.6. PMID 16382100. S2CID 17936350.
- ^ McPartland JM (2004-04-01). "Phylogenomic and chemotaxonomic analysis of the endocannabinoid system". Brain Research Reviews. 45 (1): 18–29. doi:10.1016/j.brainresrev.2003.11.005. ISSN 0165-0173. PMID 15063097. S2CID 25038370.
- ^ Paulsen CE, Armache JP, Gao Y, Cheng Y, Julius D (April 2015). "Structure of the TRPA1 ion channel suggests regulatory mechanisms". Nature. 520 (7548): 511–517. Bibcode:2015Natur.520..511P. doi:10.1038/nature14367. PMC 4409540. PMID 25855297.
- ^ Zhao J, Lin King JV, Paulsen CE, Cheng Y, Julius D (September 2020). "Irritant-evoked activation and calcium modulation of the TRPA1 receptor". Nature. 585 (7823): 141–145. Bibcode:2020Natur.585..141Z. doi:10.1038/s41586-020-2480-9. PMC 7483980. PMID 32641835. S2CID 220407248.
- ^ Basbaum AI, Bautista DM, Scherrer G, Julius D (October 2009). "Cellular and molecular mechanisms of pain". Cell. 139 (2): 267–284. doi:10.1016/j.cell.2009.09.028. PMC 2852643. PMID 19837031.
- ^ Laursen WJ, Schneider ER, Merriman DK, Bagriantsev SN, Gracheva EO (October 2016). "Low-cost functional plasticity of TRPV1 supports heat tolerance in squirrels and camels". Proceedings of the National Academy of Sciences of the United States of America. 113 (40): 11342–11347. Bibcode:2016PNAS..11311342L. doi:10.1073/pnas.1604269113. PMC 5056056. PMID 27638213.
- ^ Everaerts W, Gees M, Alpizar YA, Farre R, Leten C, Apetrei A, et al. (February 2011). "The capsaicin receptor TRPV1 is a crucial mediator of the noxious effects of mustard oil". Current Biology. 21 (4): 316–321. Bibcode:2011CBio...21..316E. doi:10.1016/j.cub.2011.01.031. PMID 21315593.
- ^ Cui M, Honore P, Zhong C, Gauvin D, Mikusa J, Hernandez G, et al. (September 2006). "TRPV1 receptors in the CNS play a key role in broad-spectrum analgesia of TRPV1 antagonists". The Journal of Neuroscience. 26 (37): 9385–9393. doi:10.1523/JNEUROSCI.1246-06.2006. PMC 6674601. PMID 16971522.
- ^ a b Huang SM, Bisogno T, Trevisani M, Al-Hayani A, De Petrocellis L, Fezza F, et al. (June 2002). "An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors". Proceedings of the National Academy of Sciences of the United States of America. 99 (12): 8400–8405. Bibcode:2002PNAS...99.8400H. doi:10.1073/pnas.122196999. PMC 123079. PMID 12060783.
- ^ Niederland V (October 1989). "[Let us be familiar with Hungarian medical literature]". Orvosi Hetilap. 130 (43): 2339. doi:10.1016/s1044-7431(03)00054-x. PMID 2812762. S2CID 23193940.
- ^ Mohapatra DP, Nau C (April 2005). "Regulation of Ca2+-dependent desensitization in the vanilloid receptor TRPV1 by calcineurin and cAMP-dependent protein kinase". The Journal of Biological Chemistry. 280 (14): 13424–13432. doi:10.1074/jbc.M410917200. PMID 15691846.
- ^ a b Khalil M, Alliger K, Weidinger C, Yerinde C, Wirtz S, Becker C, Engel MA (2018). "Functional Role of Transient Receptor Potential Channels in Immune Cells and Epithelia". Frontiers in Immunology. 9: 174. doi:10.3389/fimmu.2018.00174. PMC 5808302. PMID 29467763.
- ^ a b c d e Omari SA, Adams MJ, Geraghty DP (2017-01-01). "TRPV1 Channels in Immune Cells and Hematological Malignancies". In Geraghty DP, Rash LD (eds.). Ion Channels Down Under. Advances in Pharmacology. Vol. 79. Academic Press. pp. 173–198. doi:10.1016/bs.apha.2017.01.002. ISBN 9780128104132. PMID 28528668.
- ^ a b c d Bujak JK, Kosmala D, Szopa IM, Majchrzak K, Bednarczyk P (2019-10-16). "Inflammation, Cancer and Immunity-Implication of TRPV1 Channel". Frontiers in Oncology. 9: 1087. doi:10.3389/fonc.2019.01087. PMC 6805766. PMID 31681615.
- ^ Jacobson A, Yang D, Vella M, Chiu IM (May 2021). "The intestinal neuro-immune axis: crosstalk between neurons, immune cells, and microbes". Mucosal Immunology. 14 (3): 555–565. doi:10.1038/s41385-020-00368-1. PMC 8075967. PMID 33542493.
- ^ a b c Kong WL, Peng YY, Peng BW (August 2017). "Modulation of neuroinflammation: Role and therapeutic potential of TRPV1 in the neuro-immune axis". Brain, Behavior, and Immunity. 64: 354–366. doi:10.1016/j.bbi.2017.03.007. PMID 28342781. S2CID 4525926.
- ^ Khairatkar-Joshi N, Szallasi A (January 2009). "TRPV1 antagonists: the challenges for therapeutic targeting". Trends in Molecular Medicine. 15 (1): 14–22. doi:10.1016/j.molmed.2008.11.004. PMID 19097938.
- ^ Jhaveri MD, Elmes SJ, Kendall DA, Chapman V (July 2005). "Inhibition of peripheral vanilloid TRPV1 receptors reduces noxious heat-evoked responses of dorsal horn neurons in naïve, carrageenan-inflamed and neuropathic rats". The European Journal of Neuroscience. 22 (2): 361–370. doi:10.1111/j.1460-9568.2005.04227.x. PMID 16045489. S2CID 24664751.
- ^ Story GM, Crus-Orengo L (2008). "Feel the Burn". American Scientist. 95 (4): 326–333. doi:10.1511/2007.66.326. ISSN 0003-0996. Archived from the original on January 19, 2008.
- ^ Gunthorpe MJ, Szallasi A (2008). "Peripheral TRPV1 receptors as targets for drug development: new molecules and mechanisms". Current Pharmaceutical Design. 14 (1): 32–41. doi:10.2174/138161208783330754. PMID 18220816.
- ^ a b c Gavva NR, Bannon AW, Surapaneni S, Hovland DN, Lehto SG, Gore A, et al. (March 2007). "The vanilloid receptor TRPV1 is tonically activated in vivo and involved in body temperature regulation". The Journal of Neuroscience. 27 (13): 3366–3374. doi:10.1523/JNEUROSCI.4833-06.2007. PMC 6672109. PMID 17392452.
- ^ Steiner AA, Turek VF, Almeida MC, Burmeister JJ, Oliveira DL, Roberts JL, et al. (July 2007). "Nonthermal activation of transient receptor potential vanilloid-1 channels in abdominal viscera tonically inhibits autonomic cold-defense effectors". The Journal of Neuroscience. 27 (28): 7459–7468. doi:10.1523/JNEUROSCI.1483-07.2007. PMC 6672610. PMID 17626206.
- ^ Gavva NR (November 2008). "Body-temperature maintenance as the predominant function of the vanilloid receptor TRPV1". Trends in Pharmacological Sciences. 29 (11): 550–557. doi:10.1016/j.tips.2008.08.003. PMID 18805596.
- ^ Gavva NR, Treanor JJ, Garami A, Fang L, Surapaneni S, Akrami A, et al. (May 2008). "Pharmacological blockade of the vanilloid receptor TRPV1 elicits marked hyperthermia in humans". Pain. 136 (1–2): 202–210. doi:10.1016/j.pain.2008.01.024. PMID 18337008. S2CID 11557845.
- ^ Chizh BA, O'Donnell MB, Napolitano A, Wang J, Brooke AC, Aylott MC, et al. (November 2007). "The effects of the TRPV1 antagonist SB-705498 on TRPV1 receptor-mediated activity and inflammatory hyperalgesia in humans". Pain. 132 (1–2): 132–141. doi:10.1016/j.pain.2007.06.006. PMID 17659837. S2CID 25081522.
- ^ Szallasi A, McAlexander MA (9 April 2015). TRP channels as therapeutic targets : from basic science to clinical use. Amsterdam [Netherlands]: Elsevier Science. ISBN 978-0-12-420079-1. OCLC 912315205.
- ^ Joseph J, Qu L, Wang S, Kim M, Bennett D, Ro J, et al. (December 2019). "Phosphorylation of TRPV1 S801 Contributes to Modality-Specific Hyperalgesia in Mice". The Journal of Neuroscience. 39 (50): 9954–9966. doi:10.1523/JNEUROSCI.1064-19.2019. PMC 6978941. PMID 31676602.
- ^ Horton JS, Buckley CL, Stokes AJ (January 2013). "Successful TRPV1 antagonist treatment for cardiac hypertrophy and heart failure in mice". Channels. 7 (1): 17–22. doi:10.4161/chan.23006. PMC 3589277. PMID 23221478.
- ^ a b c Horton JS, Shiraishi T, Alfulaij N, Small-Howard AL, Turner HC, Kurokawa T, et al. (December 2019). ""TRPV1 is a component of the atrial natriuretic signaling complex, and using orally delivered antagonists, presents a valid therapeutic target in the longitudinal reversal and treatment of cardiac hypertrophy and heart failure"". Channels. 13 (1): 1–16. doi:10.1080/19336950.2018.1547611. PMC 6298697. PMID 30424709.
- ^ Pareek TK, Keller J, Kesavapany S, Agarwal N, Kuner R, Pant HC, et al. (January 2007). "Cyclin-dependent kinase 5 modulates nociceptive signaling through direct phosphorylation of transient receptor potential vanilloid 1". Proceedings of the National Academy of Sciences of the United States of America. 104 (2): 660–665. Bibcode:2007PNAS..104..660P. doi:10.1073/pnas.0609916104. PMC 1752192. PMID 17194758.
- ^ Boonen, Brett; Startek, Justyna B.; Talavera, Karel (2016-01-01). Chemical Activation of Sensory TRP Channels. Topics in Medicinal Chemistry. Springer Berlin Heidelberg. pp. 1–41. [1] doi:10.1007/7355_2015_98.
- ^ Knotkova H, Pappagallo M, Szallasi A (February 2008). "Capsaicin (TRPV1 Agonist) therapy for pain relief: farewell or revival?". The Clinical Journal of Pain. 24 (2): 142–154. doi:10.1097/AJP.0b013e318158ed9e. PMID 18209521. S2CID 31394217.
- ^ "Qutenza prescribing information" (PDF). Archived from the original (PDF) on 3 April 2018. Retrieved 23 November 2011.
- ^ a b Leishman E, Bradshaw HB (2015-01-01). "Chapter 3 - N-Acyl Amides: Ubiquitous Endogenous Cannabimimetic Lipids That Are in the Right Place at the Right Time". In Di Marzo V, Wang J (eds.). The Endocannabinoidome. Boston: Academic Press. pp. 33–48. doi:10.1016/B978-0-12-420126-2.00003-1. ISBN 978-0-12-420126-2.
- ^ Di Marzo V, Bisogno T, De Petrocellis L (July 2001). "Anandamide: some like it hot". Trends in Pharmacological Sciences. 22 (7): 346–349. doi:10.1016/s0165-6147(00)01712-0. PMID 11431028.
- ^ a b Ligresti A, Moriello AS, Starowicz K, Matias I, Pisanti S, De Petrocellis L, et al. (September 2006). "Antitumor activity of plant cannabinoids with emphasis on the effect of cannabidiol on human breast carcinoma". The Journal of Pharmacology and Experimental Therapeutics. 318 (3): 1375–1387. doi:10.1124/jpet.106.105247. PMID 16728591. S2CID 1341744.
- ^ a b De Petrocellis L, Ligresti A, Moriello AS, Allarà M, Bisogno T, Petrosino S, et al. (August 2011). "Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes". British Journal of Pharmacology. 163 (7): 1479–1494. doi:10.1111/j.1476-5381.2010.01166.x. PMC 3165957. PMID 21175579.
- ^ Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sørgård M, Di Marzo V, et al. (July 1999). "Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide". Nature. 400 (6743): 452–457. Bibcode:1999Natur.400..452Z. doi:10.1038/22761. PMID 10440374. S2CID 4301578.
- ^ Hu SS, Bradshaw HB, Benton VM, Chen JS, Huang SM, Minassi A, et al. (October 2009). "The biosynthesis of N-arachidonoyl dopamine (NADA), a putative endocannabinoid and endovanilloid, via conjugation of arachidonic acid with dopamine". Prostaglandins, Leukotrienes, and Essential Fatty Acids. 81 (4): 291–301. doi:10.1016/j.plefa.2009.05.026. PMC 2757501. PMID 19570666.
- ^ Chu CJ, Huang SM, De Petrocellis L, Bisogno T, Ewing SA, Miller JD, et al. (April 2003). "N-oleoyldopamine, a novel endogenous capsaicin-like lipid that produces hyperalgesia". The Journal of Biological Chemistry. 278 (16): 13633–13639. doi:10.1074/jbc.m211231200. PMID 12569099.
- ^ Saghatelian A, McKinney MK, Bandell M, Patapoutian A, Cravatt BF (August 2006). "A FAAH-regulated class of N-acyl taurines that activates TRP ion channels". Biochemistry. 45 (30): 9007–9015. doi:10.1021/bi0608008. PMID 16866345.
- ^ a b c d e f g Raboune S, Stuart JM, Leishman E, Takacs SM, Rhodes B, Basnet A, et al. (2014-08-01). "Novel endogenous N-acyl amides activate TRPV1-4 receptors, BV-2 microglia, and are regulated in brain in an acute model of inflammation". Frontiers in Cellular Neuroscience. 8: 195. doi:10.3389/fncel.2014.00195. PMC 4118021. PMID 25136293.
- ^ a b De Petrocellis L, Schiano Moriello A, Imperatore R, Cristino L, Starowicz K, Di Marzo V (December 2012). "A re-evaluation of 9-HODE activity at TRPV1 channels in comparison with anandamide: enantioselectivity and effects at other TRP channels and in sensory neurons". British Journal of Pharmacology. 167 (8): 1643–1651. doi:10.1111/j.1476-5381.2012.02122.x. PMC 3525867. PMID 22861649.
- ^ a b Patwardhan AM, Scotland PE, Akopian AN, Hargreaves KM (November 2009). "Activation of TRPV1 in the spinal cord by oxidized linoleic acid metabolites contributes to inflammatory hyperalgesia". Proceedings of the National Academy of Sciences of the United States of America. 106 (44): 18820–18824. doi:10.1073/pnas.0905415106. PMC 2764734. PMID 19843694.
- ^ Patwardhan AM, Akopian AN, Ruparel NB, Diogenes A, Weintraub ST, Uhlson C, et al. (May 2010). "Heat generates oxidized linoleic acid metabolites that activate TRPV1 and produce pain in rodents". The Journal of Clinical Investigation. 120 (5): 1617–1626. doi:10.1172/JCI41678. PMC 2860941. PMID 20424317.
- ^ Sisignano M, Angioni C, Ferreiros N, Schuh CD, Suo J, Schreiber Y, et al. (2013). "Synthesis of lipid mediators during UVB-induced inflammatory hyperalgesia in rats and mice". PLOS ONE. 8 (12): e81228. Bibcode:2013PLoSO...881228S. doi:10.1371/journal.pone.0081228. PMC 3857181. PMID 24349046.
- ^ Mabalirajan U, Rehman R, Ahmad T, Kumar S, Singh S, Leishangthem GD, et al. (2013). "Linoleic acid metabolite drives severe asthma by causing airway epithelial injury". Scientific Reports. 3: 1349. Bibcode:2013NatSR...3E1349M. doi:10.1038/srep01349. PMC 3583002. PMID 23443229.
- ^ Wen H, Östman J, Bubb KJ, Panayiotou C, Priestley JV, Baker MD, Ahluwalia A (April 2012). "20-Hydroxyeicosatetraenoic acid (20-HETE) is a novel activator of transient receptor potential vanilloid 1 (TRPV1) channel". The Journal of Biological Chemistry. 287 (17): 13868–13876. doi:10.1074/jbc.M111.334896. PMC 3340178. PMID 22389490.
- ^ Gregus AM, Doolen S, Dumlao DS, Buczynski MW, Takasusuki T, Fitzsimmons BL, et al. (April 2012). "Spinal 12-lipoxygenase-derived hepoxilin A3 contributes to inflammatory hyperalgesia via activation of TRPV1 and TRPA1 receptors". Proceedings of the National Academy of Sciences of the United States of America. 109 (17): 6721–6726. Bibcode:2012PNAS..109.6721G. doi:10.1073/pnas.1110460109. PMC 3340022. PMID 22493235.
- ^ Gregus AM, Dumlao DS, Wei SC, Norris PC, Catella LC, Meyerstein FG, et al. (May 2013). "Systematic analysis of rat 12/15-lipoxygenase enzymes reveals critical role for spinal eLOX3 hepoxilin synthase activity in inflammatory hyperalgesia". FASEB Journal. 27 (5): 1939–1949. doi:10.1096/fj.12-217414. PMC 3633813. PMID 23382512.
- ^ Pace-Asciak CR (April 2015). "Pathophysiology of the hepoxilins". Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids. 1851 (4): 383–396. doi:10.1016/j.bbalip.2014.09.007. PMID 25240838.
- ^ "Reference SNP (refSNP) Cluster Report: Rs11209716".
- ^ Maher SA, Dubuis ED, Belvisi MG (June 2011). "G-protein coupled receptors regulating cough". Current Opinion in Pharmacology. 11 (3): 248–253. doi:10.1016/j.coph.2011.06.005. PMID 21727026.
- ^ Grilo A, Sáez-Rosas MP, Santos-Morano J, Sánchez E, Moreno-Rey C, Real LM, et al. (January 2011). "Identification of genetic factors associated with susceptibility to angiotensin-converting enzyme inhibitors-induced cough". Pharmacogenetics and Genomics. 21 (1): 10–17. doi:10.1097/FPC.0b013e328341041c. PMID 21052031. S2CID 22282464.
- ^ Qu Q, Xuan W, Fan GH (January 2015). "Roles of resolvins in the resolution of acute inflammation". Cell Biology International. 39 (1): 3–22. doi:10.1002/cbin.10345. PMID 25052386. S2CID 10160642.
- ^ Serhan CN, Chiang N, Dalli J, Levy BD (October 2014). "Lipid mediators in the resolution of inflammation". Cold Spring Harbor Perspectives in Biology. 7 (2): a016311. doi:10.1101/cshperspect.a016311. PMC 4315926. PMID 25359497.
- ^ Lim JY, Park CK, Hwang SW (2015). "Biological Roles of Resolvins and Related Substances in the Resolution of Pain". BioMed Research International. 2015: 830930. doi:10.1155/2015/830930. PMC 4538417. PMID 26339646.
- ^ Ji RR, Xu ZZ, Strichartz G, Serhan CN (November 2011). "Emerging roles of resolvins in the resolution of inflammation and pain". Trends in Neurosciences. 34 (11): 599–609. doi:10.1016/j.tins.2011.08.005. PMC 3200462. PMID 21963090.
- ^ Serhan CN, Chiang N, Dalli J (May 2015). "The resolution code of acute inflammation: Novel pro-resolving lipid mediators in resolution". Seminars in Immunology. 27 (3): 200–215. doi:10.1016/j.smim.2015.03.004. PMC 4515371. PMID 25857211.
- ^ "N-Oleoyl Dopamine (CAS 105955-11-1)". www.caymanchem.com.
- ^ Ross RA (November 2003). "Anandamide and vanilloid TRPV1 receptors". British Journal of Pharmacology. 140 (5): 790–801. doi:10.1038/sj.bjp.0705467. PMC 1574087. PMID 14517174.
- ^ Högestätt ED, Jönsson BA, Ermund A, Andersson DA, Björk H, Alexander JP, et al. (September 2005). "Conversion of acetaminophen to the bioactive N-acylphenolamine AM404 via fatty acid amide hydrolase-dependent arachidonic acid conjugation in the nervous system". The Journal of Biological Chemistry. 280 (36): 31405–31412. doi:10.1074/jbc.M501489200. PMID 15987694.
- ^ a b Starkus J, Jansen C, Shimoda LM, Stokes AJ, Small-Howard AL, Turner H (December 2019). "Diverse TRPV1 responses to cannabinoids". Channels. 13 (1): 172–191. doi:10.1080/19336950.2019.1619436. PMC 6557596. PMID 31096838.
- ^ Morales P, Hurst DP, Reggio PH (2017). "Molecular Targets of the Phytocannabinoids: A Complex Picture". Phytocannabinoids. Progress in the Chemistry of Organic Natural Products. Vol. 103. pp. 103–131. doi:10.1007/978-3-319-45541-9_4. ISBN 978-3-319-45539-6. PMC 5345356. PMID 28120232.
- ^ Jansen C, Shimoda LM, Kawakami JK, Ang L, Bacani AJ, Baker JD, et al. (December 2019). "Myrcene and terpene regulation of TRPV1". Channels. 13 (1): 344–366. doi:10.1080/19336950.2019.1654347. PMC 6768052. PMID 31446830.
- ^ Long W, Johnson J, Kalyaanamoorthy S, Light P (December 2021). "TRPV1 channels as a newly identified target for vitamin D". Channels. 15 (1): 360–374. doi:10.1080/19336950.2021.1905248. PMC 8032246. PMID 33825665.
- ^ Starowicz K, Cristino L, Di Marzo V (2008). "TRPV1 receptors in the central nervous system: potential for previously unforeseen therapeutic applications". Current Pharmaceutical Design. 14 (1): 42–54. doi:10.2174/138161208783330790. PMID 18220817.
- ^ a b Gibson HE, Edwards JG, Page RS, Van Hook MJ, Kauer JA (March 2008). "TRPV1 channels mediate long-term depression at synapses on hippocampal interneurons". Neuron. 57 (5): 746–759. doi:10.1016/j.neuron.2007.12.027. PMC 2698707. PMID 18341994.
- ^ Peters JH, McDougall SJ, Fawley JA, Smith SM, Andresen MC (March 2010). "Primary afferent activation of thermosensitive TRPV1 triggers asynchronous glutamate release at central neurons". Neuron. 65 (5): 657–669. doi:10.1016/j.neuron.2010.02.017. PMC 2837850. PMID 20223201.
- ^ Numazaki M, Tominaga T, Takeuchi K, Murayama N, Toyooka H, Tominaga M (June 2003). "Structural determinant of TRPV1 desensitization interacts with calmodulin". Proceedings of the National Academy of Sciences of the United States of America. 100 (13): 8002–8006. Bibcode:2003PNAS..100.8002N. doi:10.1073/pnas.1337252100. PMC 164702. PMID 12808128.
- ^ a b Morenilla-Palao C, Planells-Cases R, García-Sanz N, Ferrer-Montiel A (June 2004). "Regulated exocytosis contributes to protein kinase C potentiation of vanilloid receptor activity". The Journal of Biological Chemistry. 279 (24): 25665–25672. doi:10.1074/jbc.M311515200. PMID 15066994.
- ^ a b Fonseca BM, Correia-da-Silva G, Teixeira NA (May 2018). "Cannabinoid-induced cell death in endometrial cancer cells: involvement of TRPV1 receptors in apoptosis". Journal of Physiology and Biochemistry. 74 (2): 261–272. doi:10.1007/s13105-018-0611-7. PMID 29441458. S2CID 25294779.
- ^ Heyman I, Rang HP (May 1985). "Depolarizing responses to capsaicin in a subpopulation of rat dorsal root ganglion cells". Neuroscience Letters. 56 (1): 69–75. doi:10.1016/0304-3940(85)90442-2. PMID 4011050. S2CID 42235338.
Further reading
edit- Premkumar LS, Ahern GP (December 2000). "Induction of vanilloid receptor channel activity by protein kinase C". Nature. 408 (6815): 985–990. Bibcode:2000Natur.408..985P. doi:10.1038/35050121. PMID 11140687. S2CID 4372628.
- Immke DC, Gavva NR (October 2006). "The TRPV1 receptor and nociception". Seminars in Cell & Developmental Biology. 17 (5): 582–591. doi:10.1016/j.semcdb.2006.09.004. PMID 17196854.
- Heiner I, Eisfeld J, Lückhoff A (2004). "Role and regulation of TRP channels in neutrophil granulocytes". Cell Calcium. 33 (5–6): 533–540. doi:10.1016/S0143-4160(03)00058-7. PMID 12765698.
- Geppetti P, Trevisani M (April 2004). "Activation and sensitisation of the vanilloid receptor: role in gastrointestinal inflammation and function". British Journal of Pharmacology. 141 (8): 1313–1320. doi:10.1038/sj.bjp.0705768. PMC 1574908. PMID 15051629.
- Szallasi A, Cruz F, Geppetti P (November 2006). "TRPV1: a therapeutic target for novel analgesic drugs?". Trends in Molecular Medicine. 12 (11): 545–554. doi:10.1016/j.molmed.2006.09.001. PMID 16996800.
- Pingle SC, Matta JA, Ahern GP (2007). "Capsaicin Receptor: TRPV1 a Promiscuous TRP Channel". Transient Receptor Potential (TRP) Channels. Handbook of Experimental Pharmacology. Vol. 179. pp. 155–71. doi:10.1007/978-3-540-34891-7_9. ISBN 978-3-540-34889-4. PMID 17217056.
- Liddle RA (August 2007). "The role of Transient Receptor Potential Vanilloid 1 (TRPV1) channels in pancreatitis". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1772 (8): 869–878. doi:10.1016/j.bbadis.2007.02.012. PMC 1995747. PMID 17428642.
External links
edit- Vanilloid+receptors at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- Overview of all the structural information available in the PDB for UniProt: O35433 (Rat Transient receptor potential cation channel subfamily V member 1) at the PDBe-KB.
- The Endocannabinoidome The World of Endocannabinoids and Related Mediators Book • 2014